Don't Let Achilles Tendinopathy Affect Your Athletic Performance



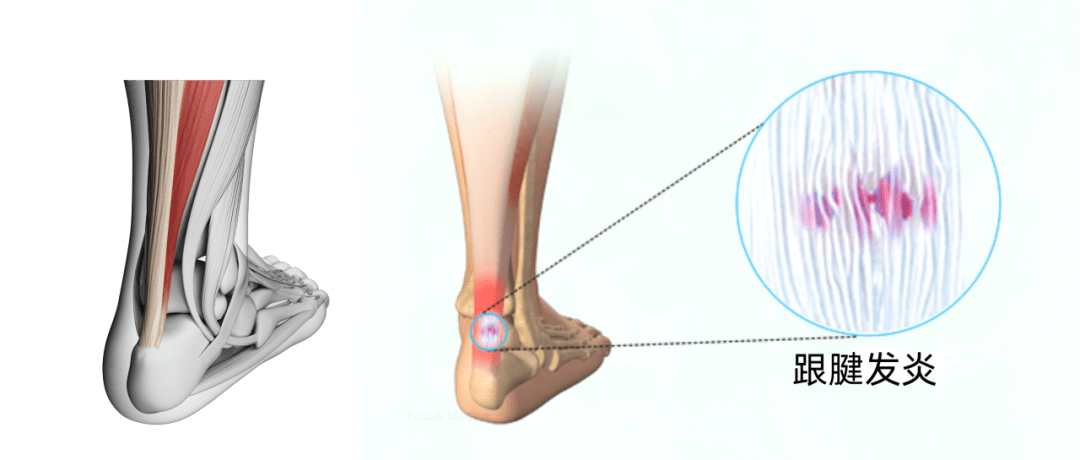
Achilles tendinopathy is a common condition affecting both active and sedentary individuals. The Achilles tendon is the largest and strongest tendon in the human body, connecting the gastrocnemius and soleus muscles to the calcaneus. The Achilles tendon plays a crucial role in plantar flexion of the ankle, a movement that is essential for walking and running. The tendons making up the Achilles are not parallel but start to twist as they run down from the mid-calf to the calcaneus, forming a coiled structure. Overuse or excessive stress on the achilles tendon can lead to inflammation or degeneration, resulting in Achilles tendinopathy.

Author / Connie Li
UP Medical
Types of Achilles Tendinopathy
●Based on the location of theinjury, Achilles tendinopathy can be classified into insertional and mid-portion tendinopathy. Research indicates the area most susceptible to injury is 2-6 cm above the insertion point at the calcaneus, characterized by poor blood supply and a smaller cross-sectional area.
●- Insertional Achilles Tendinopathy: Located at the junction of the Achilles tendon and the calcaneus.
●- Mid-portion Achilles Tendinopathy: 2-6 cm above the calcaneus.
Prevalence of Achilles Tendinopathy
According to clinical guidelines for Achilles tendinopathy, which was published in 2018 by the authoritative institution APTA:
●The prevalence of Achilles tendinopathy in elite male soccer players during 1 season ranged from 2.1% to 5.1%.
●In a large prospective cohort of novice runners, 7% went on to develop Achilles tendinopathy.
●In a systematic review, reported prevalence of Achilles tendinopathy in the general running and ultramarathon populations ranged from 6.2% to 9.5% and 2.0% to 18.5%, respectively.
●Achilles tendinopathy was found to occur in 12.5% of rock climbers.
● With age, the incidence of Achilles tendon injuries increases, averaging between 30-50 years.

Risk Factors for Achilles Tendinopathy
Intrinsic Factors:
●- Ankle dorsiflexion range of motion
●- Abnormal subtalar joint motion
●- Decreased ankle plantarflexion strength
●- Excessive foot pronation
●- Abnormal Achilles tendon structure
●- Comorbidities (the presence of two or more diseases or medical conditions in a patient): obesity,hypertension, hypercholesterolemia, diabetes, systemic inflammatory arthritis
Extrinsic Factors:
●- Training: increased mileage,intensity, hill training, rapid return to training after rest,etc.
●- Environmental: lower temperatures
●- Equipment: inappropriate gear,orthotics, etc.
Other Causes of Heel Pain
●Besides Achilles tendinopathy,other injuries can cause heel pain, such as:
●- Acute Achilles tendon rupture
●- Partial tear of the Achilles tendon
●- Retrocalcaneal bursitis
●- Posterior ankle impingement
●- Irritation or neuroma of the sural nerve
●- Ostrigonum syndrome
●- Accessory soleus muscle injury
●- Achilles tendon ossification
●- Systemic inflammatory disease
How to diagnose Achilles tendinopathy? Try the following screening methods.
Arc test:Test is positive for Achilles tendinopathy if the area of swelling moves with dorsiflexion and plantarflexion. To test for this, the:
1.Patient lies prone with ankles off the table.
2.Clinician palpates Achilles tendon 2-6 cm above calcaneus,gently squeezing between the thumb and index finger to feel for localized thickening
3.Patient dorsiflexes and plantarflexes; observe if swelling moves.

Royal London Hospital test:
Test is positive for Achilles tendinopathy if initial tenderness is absent in maximum dorsiflexion position. To test for this, the:
1.Patient lies prone with ankles off the table.
2.Clinician palpates Achilles tendon for tenderness (2-5 cm from calcaneal insertion),gently squeezing between thumb and index finger
3.While palpating the tender spot, the patient performs slight ankle dorsiflexion
4.Patient maximally plantarflexes; palpates tender spot again


Imaging for Achilles Tendinopathy
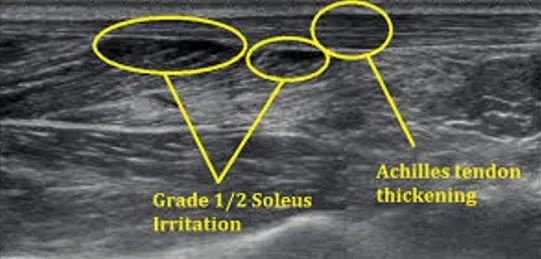
●Ultrasound is considered the gold standard for diagnosing Achilles tendinopathy. Fredberg et al. found that ultrasound could detect Achilles tendinopathy before the onset of pain. In a study of 96 asymptomatic professional soccer players (18-35 years), 11% showed abnormal signals before the season. By the end of the season, 45% experienced Achilles pain, compared to only 1% with initially nomal signals.
Treatment for Achilles Tendinopathy
●Despite increasing research, the optimal treatment for Achilles tendinopathy remains debated. Conservative treatment is typically preferred, but surgery may be considered if it fails.Treatment plans should be tailored to the patient’s needs and activity levels.
●Main treatment methods accordingto APTA guidelines include: Exercise therapy、Stretching、Neuromuscular re-education、Extracorporeal shock wave therapy、Joint mobility improvement、Taping、Dry needling、Corticosteroid injections、Patient education (injury mechanisms, risk factor adjustment, rehabilitation time)
Exercise therapy
●Eccentric exercise is currently considered the most effective therapeutic approach, especially high-resistance and slow-speed eccentric training. However,Cook JL suggests that eccentric training is not suitable for every patient, and the prerequisite for eccentric exercise is the absence of structural frailty in the Achilles tendon.)

●Towel Grab Exercise(Crowley’s 2019 study showed that patients with insertional Achilles tendinopathy have significantly lower plantar flexion strength on both the affected and unaffected sides compared to those with non-insertional Achilles tendinopathy.)
●Utilize the intrinsic foot muscles to grab the towel, employing not only the hallux but also the other toe extensors.
●Heel Raise with Ball Squeeze Exercise:Strengthen the Tibialis Posterior


●Weighted Ball Carry Walk:
Strengthen the stability of the ankle joint in dorsiflexion and plantarflexion.
●Ankle Resistance Band Training:Strengthen the muscles responsible for ankle eversion and inversion.


Self-Myofascial Release
●Standing Calf Stretch Against the Wall
●Using a fascia ball to release the calf muscles
●Plantar Fascia Release



Joint Mobility Training:
●If you find your dorsiflexion range limited and stretching the calf muscles doesn’t improve it, it may be due to talus impingement. Please try ankle joint mobility exercises.


Prevention of Achilles Tendinopathy
●Gradually increase training volume to avoid sudden increases in distance and intensity.
●Proper warm-up and stretching,especially for calf muscles, to enhance flexibility and joint range of motion.
●Improve running posture: Ensure correct running and walking posture to reduce unnecessary tendon stress. For example, avoid excessive pronation or supination during running.
●Choose appropriate footwear providing arch support and stability.
● Strengthen the calf muscles through muscle strength and balance training to reduce strain on the Achilles tendon.
●Seek medical attention for chronic pain to prevent further issues.
●Allow sufficient rest and recovery after exercise, ensuring good sleep and nutrition.
●Regular check-ups: Undergo regular physical examinations and sports assessments to monitor the health of muscles and tendons, and to identify and address issues early on.
References:
●Carcia C R, Martin R L, Houck J, et al.Achilles pain, stiffness, and muscle power deficits: achilles tendinitis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the Orthopaedic Section of the American Physical Therapy Association[J]. Journal of Orthopaedic& Sports Physical Therapy, 2010, 40(9): A1-A26.
●Achilles Pain, Stiffness, and Muscle Power Deficits: Midportion Achilles Tendinopathy Revision 2018 Robroy L.Martin, Ruth Chimenti,Tyler Cuddeford,Jeff Houck, J.W. Matheson, Christine M. McDonough, Stephen Paulseth,Dane K. Wukich,and Christopher R. Carcia Journal of Orthopaedic& Sports Physical Therapy 2018 48:5, A1-A38
●Krolo I, Viskovic K, Ikic D, Klaric-Custovic R, MarottiM, Cicvara T. Therisk of sports activities–the injuries of the Achilles tendon in sportsmen.Coll Antropol.2007;31:275-278
●Pękala PA, Henry BM, Ochała A,et al. The twisted structure of the Achilles tendon unraveled: A detailed quantitative and qualitative anatomical investigation. Scand JMed Sci Sports. 2017: 27: 1705–1715. https://doi.org/10.1111/sms.12835

本篇文章來源于微信公衆号: 上海優複康複醫學門診部

